
(616) 846-3400
Fax: (616) 846-3406

(616) 846-3400
Fax: (616) 846-3406

Being a parent involves caring for your child in every way you can. You make sure they are eating the right food, being nice to others, and staying out of any trouble. However, it is also important that you are watchful of their health, more specifically their foot health. Maintaining good foot health in childhood is important in preventing later conditions in life from happening. As children continue to develop, their feet require different techniques of care. Here are some various ways in which you can help your child’s feet stay healthy.
A baby needs a lot of care and attention overall, but the importance of their feet should never be forgotten. Before a baby turns one, their feet change and develop greatly. It is important that during this time, a mother avoids putting tight socks on their child. She should also encourage movement of their feet so the baby can begin to feel more comfortable using them.
As a baby enters the toddler years of his or her life, they are begin to walk around. When your baby begins to take those first steps, it is crucial that they are wearing protective shoes on their feet. As a mother that is observant of your child’s feet, you may notice changes in them. This is completely normal as the feet are becoming susceptible to the activity of walking. It is normal for a toddler to be a bit unsteady or to “walk funny” at first.
When your child grows out of their toddler years, it is important that you begin to show him or her how to care for their feet on their own. Practice with your child proper hygiene in order to prevent foot fungus or infection. Since children are constantly on the move, it is crucial to be cautious of any accidents or injuries that might occur. If an injury occurs, it is advised that you take your child to be examined by a doctor immediately. Since your child is still growing, particular injuries can shift the way in which a bone or other important part of the foot is developing.
Babies and kids are always changing and growing. Your job as a parent is to make sure they stay healthy and making sure they are properly maintained. This involves proper foot care and making sure the feet stay healthy. Following this guide, your child can live a long and happy life.

Osteoarthritis, or OA, which is often associated with aging and wear-and-tear, isn't limited to just the knees and hips. It can also affect the ankle joint, causing pain and mobility issues. Osteoarthritis in the ankle is a chronic condition that develops when the protective cartilage that cushions the bones begins to deteriorate. OA can occur at any time of life, but it is most common in older adults. Being overweight adds stress to your ankles and fat cells produce proteins that may make the condition worse. Any ankle injury, even one that happened years ago, can lead to osteoarthritis. Symptoms include pain, stiffness, swelling, and a reduced range of motion, which can significantly affect your daily life. Even simple tasks like walking and climbing stairs can become challenging. Several factors can contribute to ankle osteoarthritis, including previous injuries, genetics, and obesity. Treatment options include medication, physical therapy, orthotic devices, and in some cases, surgery. Osteoarthritis is a progressive disease, and for that reason managing it requires a comprehensive approach to reduce pain and maintain mobility. It's suggested that you make an appointment with a podiatrist if you suspect osteoarthritis is affecting your ankles.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Dr. Robbi Young from Grand Haven Foot & Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact our office located in Grand Haven, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Arthritis is an inflammation of the joints and it can occur at any joint in the body, especially in the foot. It generally effects those who are older, however, it can occur at any age. Although there are many different forms of arthritis, there are three main types that occur in the foot. The three types are osteoarthritis, rheumatoid arthritis, and gout.
The primary cause of osteoarthritis is aging. As you age, cartilage degenerates around the joints which causes friction and pain. Obesity can cause osteoarthritis through mechanical stress. Injuries that damage joints can increase the probability as well. Finally, a family history of osteoarthritis can also increase chances of having it.
Rheumatoid arthritis occurs when the immune system attacks the joint linings and weakens them over a long time. While there is no known cause of rheumatoid arthritis, obesity and smoking can increase your chances of getting it. Women are also more likely to get it than men.
Gout is a form of arthritis that occurs when there is too much uric acid in your blood and painful crystals form in your joints. Men are more likely to have gout than women. People who are obese or drink alcohol often are also more likely to develop gout. Furthermore, having diabetes, heart disease, high blood pressure, high cholesterol, gastric bypass surgery or a family history of gout may increase your likelihood of developing the condition.
Symptoms of arthritis include pain, stiffness, swelling in the joints. These symptoms can make it harder and more painful to walk. Physical activity can increase pain and discomfort. Furthermore, joint pain can worsen throughout the day for osteoarthritis. Gout attacks generally last several days with the first few being the worst.
Diagnosis of gout includes either a joint fluid test or a blood test. X-ray imaging can detect osteoarthritis but not gout. On the other hand, there is no blood test for osteoarthritis. Rheumatoid arthritis is difficult to diagnosis. Doctors utilize family and personal medical history, a physical examination, and antibody blood tests to determine if you have rheumatoid arthritis.
Treatment varies for the different kinds of arthritis. Anti-inflammatory medication or steroids can help reduce pain from inflammation of the joints. Changing shoe types can help with some symptoms. Wider shoes can help with discomfort from gout and osteoarthritis. High heels should be avoided. Shoes with proper arch support and that take pressure off the ball of the foot can help with rheumatoid arthritis. Drinking lots of water can also help rid uric acid from the blood. Losing weight, improving your diet, and limiting alcohol and smoking can also help prevent or lessen the symptoms of arthritis.
If you are having trouble walking or pain in your feet, see a podiatrist to check if you have arthritis.

Flat feet, also known as fallen arches, is a common condition where the arches of the feet appear to be flat or absent. Understanding the anatomy of flat feet can shed light on this condition. The arch of the foot is a vital structural feature, composed of tendons, ligaments, and bones, including the tarsal and metatarsal bones. In individuals with normal arches, these structures work together to absorb shock, distribute weight, and provide stability during movement. However, in individuals with flat feet, these components may not function as effectively. Common causes of flat feet include genetics, injury, or conditions such as tendon dysfunction. When the arch collapses or flattens, it can result in an uneven distribution of weight on the foot, leading to pain, fatigue, and potential musculoskeletal issues. Understanding the anatomy of flat feet is the first step towards seeking appropriate care and management. It is suggested that you consult with a podiatrist who can help individuals with flat feet explore treatment options. These can include wearing orthotics, doing specific exercises, and, in some cases, undergoing surgery to address discomfort and improve foot function.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Dr. Robbi Young from Grand Haven Foot & Ankle. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Grand Haven, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flatfoot is a foot condition in which the arch of the foot has either partially or totally dropped or has never developed. While it is common in babies and small children, it can become a problem for them in adulthood if the arch never forms. For adults, the development of flat feet can be brought upon by injury, as a result of pregnancy due to increased elasticity, or obesity. Those who have health concerns such as rheumatoid arthritis or diabetes may also be at greater risk for developing the condition.
If you suspect that you have flat feet, it is best to consult your podiatrist. Your foot doctor will examine the suspected foot and observe how it looks while you sit and stand. He or she may take an X-ray to determine how serious the condition is. Some common signs of flatfoot include toe drift, in which the toes and front part of the foot point outward, a short Achilles tendon, and a heel that tilts outwardly while the ankle tilts inward.
Once flatfoot has been diagnosed, your podiatrist may suggest one of several treatment options. Flat feet can be rigid, in which the feet appear to have no arch even when the person is not standing; or flexible, in which the person appears to have an arch while not standing, but once standing the arch disappears. Those with flexible flatfoot may be told to reduce any activities that cause pain and to avoid extended periods of walking or standing. Another suggestion may be weight loss, as excessive weight may be placing pressure on the arches
In few cases, if the condition is severe and all other methods have been exhausted surgery may be required. This is normally avoided, however, due to a lengthy recovery time and high cost.

A broken toe can happen to anyone, whether it is from a sudden accident or a simple misstep. The first step in treating a broken toe is recognizing the signs. Pain, swelling, bruising, and difficulty in moving the toe are common indicators. If you suspect a break, it is essential to seek medical attention promptly. To confirm the broken toe, a diagnosis is often needed by having an X-ray taken. In the meantime, you can take some steps to alleviate discomfort. Resting the affected foot and elevating it may help to reduce swelling. Immobilize the toe by buddy-taping it to an adjacent healthy toe, which can provide support and stability during the healing process. Taking over-the-counter pain relievers can help to manage pain, and it is helpful to avoid putting weight on the injured toe. If the fracture is severe or displaced, the toe may need to be reset or placed in a splint. Healing a broken toe takes time, so it is advised to be patient and take good care of your injured toe. If you have broken your toe, it is suggested that you visit a podiatrist who can effectively diagnose and treat this injury.
A broken toe can be very painful and lead to complications if not properly fixed. If you have any concerns about your feet, contact Dr. Robbi Young from Grand Haven Foot & Ankle. Our doctor will treat your foot and ankle needs.
What to Know About a Broken Toe
Although most people try to avoid foot trauma such as banging, stubbing, or dropping heavy objects on their feet, the unfortunate fact is that it is a common occurrence. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break (fracture).
Symptoms of a Broken Toe
Generally, it is best to stay off of the injured toe with the affected foot elevated.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery. Due to its position and the pressure it endures with daily activity, future complications can occur if the big toe is not properly treated.
If you have any questions please feel free to contact our office located in Grand Haven, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Trauma to the foot, especially the toes, can occur in many ways. Banging them, stubbing them, or dropping something on them are a few different ways this trauma can occur. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break or fracture. Another type of trauma that can break a toe is repeated activity that places stress on the toe for prolonged periods of time.
Broken toes can be categorized as either minor or severe fractures. Symptoms of minor toe fractures include throbbing pain, swelling, bruising on the skin and toenail, and the inability to move the toe with ease. Severe toe fractures require medical attention and are indicated when the broken toe appears crooked or disfigured, when there is tingling or numbness in the toe, or when there is an open, bleeding wound present on the toe.
Generally, a minor toe break will heal without long-term complications. However, it is important to discontinue activities that put pressure on the toe. It is best to stay off of the injured toe and immediately get a splint or cast to prevent any more additional movement of the toe bones. You can also immobilize your toe by placing a small cotton ball between the injured toe and the toe beside it. Then, tape the two toes together with medical tape. Swelling can be alleviated by placing an ice pack on the broken toe directly as well as elevating your feet above your head.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery, especially when the big toe has been broken. Due to its position and the pressure the big toe endures with daily activity, future complications can occur if it is not properly treated. Pain associated with minor toe fractures can be managed with over-the-counter pain medications. Prescription pain killers may be necessary for severe toe fractures.
The healing time for a broken toe is approximately four to six weeks. In severe cases where the toe becomes infected or requires surgery, healing time can take up to eight weeks or more. While complications associated with a broken toe are immediately apparent, it is important to note that there are rare cases when additional complications, such as osteoarthritis, can develop over time. You should immediately speak with your podiatrist if you think you have broken your toe due to trauma. They will be able to diagnose the injury and recommend the appropriate treatment options.
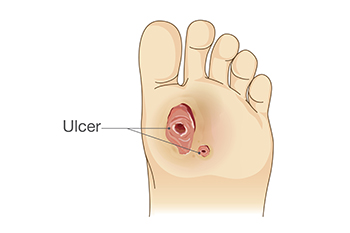
Diabetes affects the body's ability to heal foot wounds due to its impact on metabolizing glucose. High blood sugar levels hinder wound healing by preventing efficient nutrient and oxygen delivery, reducing immune system function, and increasing inflammation. Peripheral neuropathy, common in diabetes, can lead to reduced sensation in the feet, making foot wounds more prevalent. Poor circulation, often linked to diabetes, further impairs healing by reducing blood flow and affecting red blood cell function. Immune system deficiencies in diabetes hinder the body's ability to heal foot wounds and increase the risk of infection. Elevated blood sugar levels also promote bacterial growth, worsening the risk of infection. To aid in foot wound healing, performing regular self-foot checks are crucial in detecting wounds early. Removing dead tissue, keeping dressings fresh, and avoiding pressure on the wound can facilitate healing. If you experience symptoms such as tingling, burning, or persistent pain, or if your foot wound worsens, it is suggested that you make an appointment with a podiatrist as quickly as possible who can help you manage this serious condition.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Robbi Young from Grand Haven Foot & Ankle. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Grand Haven, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.